Health News
View All
Your Spouse’s Stroke Could Increase Your Depression Risk
The spouses of people who have strokes, heart attacks, and heart failure are more likely to experience depression than people whose spouses didn’t have those health problems, a new study shows.
Mobile Medical Units Bringing Cancer Screenings Where it's Needed
Don’t Worry, Gen Z, Your Face Isn’t Aging Faster Than Others
The Fat You Can’t See Can Be Most Dangerous to Your Health
Special Section
 Content on Myasthenia Gravis
Content on Myasthenia GravisCreating a Plan for Your Treatment and Well-Being
Find out how to build a treatment plan with your doctor plus how to manage your overall health while living with myasthenia gravis.
 Spotlight on Medicare Advantage
Spotlight on Medicare AdvantageDiscover How You Can Make the Most of Medicare Advantage
From making your prior authorization process easier to understanding your prescription coverage, what to know.
 Spotlight on a Clean Home
Spotlight on a Clean HomeHow Clean Is Your House?
Learn how to beat germs and improve air quality in every room of your home.
Free WebMD Newsletters
Doctor-approved health and wellness information delivered to your inbox.

Patient and Expert Contributors
View All- Substance Abuse & Addiction
 Ashley WalkerDiagnosed since 2010
Ashley WalkerDiagnosed since 2010 - Health Topics A-Z
 Lyric PorterDiagnosed since 1996
Lyric PorterDiagnosed since 1996 - Digestive Problems
 Elizabeth Ward, RD, MSRegistered dietitian nutritionist
Elizabeth Ward, RD, MSRegistered dietitian nutritionist - Digestive Problems
 Sally Kuzemchak, RD, MSRegistered dietitian
Sally Kuzemchak, RD, MSRegistered dietitian
Health A - Z
View AllADD/ADHD - Childhood
ADHD
Allergies
Alzheimer's
Ankylosing Spondylitis
Anxiety Disorders
Arthritis
Asthma
Back Pain
Cancer
Children's Vaccines
Cholesterol
Cold, Flu, & Cough
COPD
Coronavirus
Depression
Diabetes
Digestive Disorders
Eye Health
Health & Balance
Heart Health
Heartburn/GERD
Hypertension
Lung Cancer
Mental Health
Migraines
Multiple Myeloma
Multiple Sclerosis
Oral Care
Orthopedics
Osteoporosis
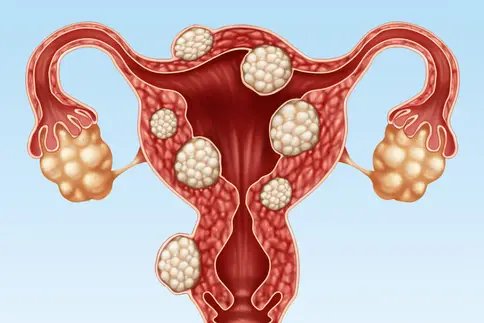
Ovarian Cancer
Prostate Cancer
Psoriasis
Rheumatoid Arthritis
Schizophrenia
Sexual Conditions
Skin Problems
Sleep Disorders
Our Content Is Different Because We Set the Bar Higher
As a leader in digital health publishing for more than 25 years, WebMD strives to maintain the most comprehensive and reliable source of health and medical information on the internet.
We recognize the responsibility that comes along with being the most well-known and trusted health information platform — and we take that responsibility seriously by:
- 01Charging our content creators to practice journalistic principles of excellence and provide objective, accurate, and balanced reporting
- 02Maintaining editorial independence and transparency into how we protect the integrity of our content
- 03Regularly reviewing and updating our content by working with our network of more than 100 doctors and health experts